
As the COVID-19 virus continues to spread across the globe, more people are taking steps to flatten the curve, reduce the spread, and prevent the virus from overwhelming the healthcare system. This has led to an increase in handwashing and purchasing of hand sanitizer, but more people are also beginning to understand the importance of face masks. Learn more about face masks and the best type of face masks to protect against the COVID-19 virus.
How Face Masks Work
When you cough, sneeze, talk, or even just breathe, you expel air and microscopic water droplets that can potentially carry viral microbes into the area around you. The smallest of these droplets are sometimes referred to as aerosols. These tiny droplets are light enough to hang in the air for hours and potentially expose anyone who walks through that airspace to the virus.1
This is why most experts recommend staying at least 6 feet away from others to minimize exposure to these droplets. However, some studies suggest that an uncovered sneeze can potentially create droplets that travel up to 27 feet before falling to the ground or other surfaces.2
Face masks cover the mouth and nose, which helps to prevent the spread of infection three ways. First, it keeps those who are infected from infecting others by stifling droplets, minimizing the number of droplets that actually make it into the air as well as the distance that those droplets go. Secondly, masks protect the uninfected from breathing in potentially viral droplets hanging in the air. Lastly, face masks aren’t just a physical barrier for droplets. They can physically alter the habit of face touching, which is one of the most common ways of transferring viruses and other microbes on the hands to the mouth, nose, or eyes.1
The Best Face Masks
While face masks have been shown to work, they are not all created equal. This mainly comes down to the size of the droplets that they can filter out. For example, the average size of a SARS-causing coronavirus measures roughly 0.08 to 0.14 microns, so having a mask with a filter smaller than that naturally prevents the virus from even getting to you.3 Learn more about common face masks below.
*We now offer hand sanitizers. Click HERE*
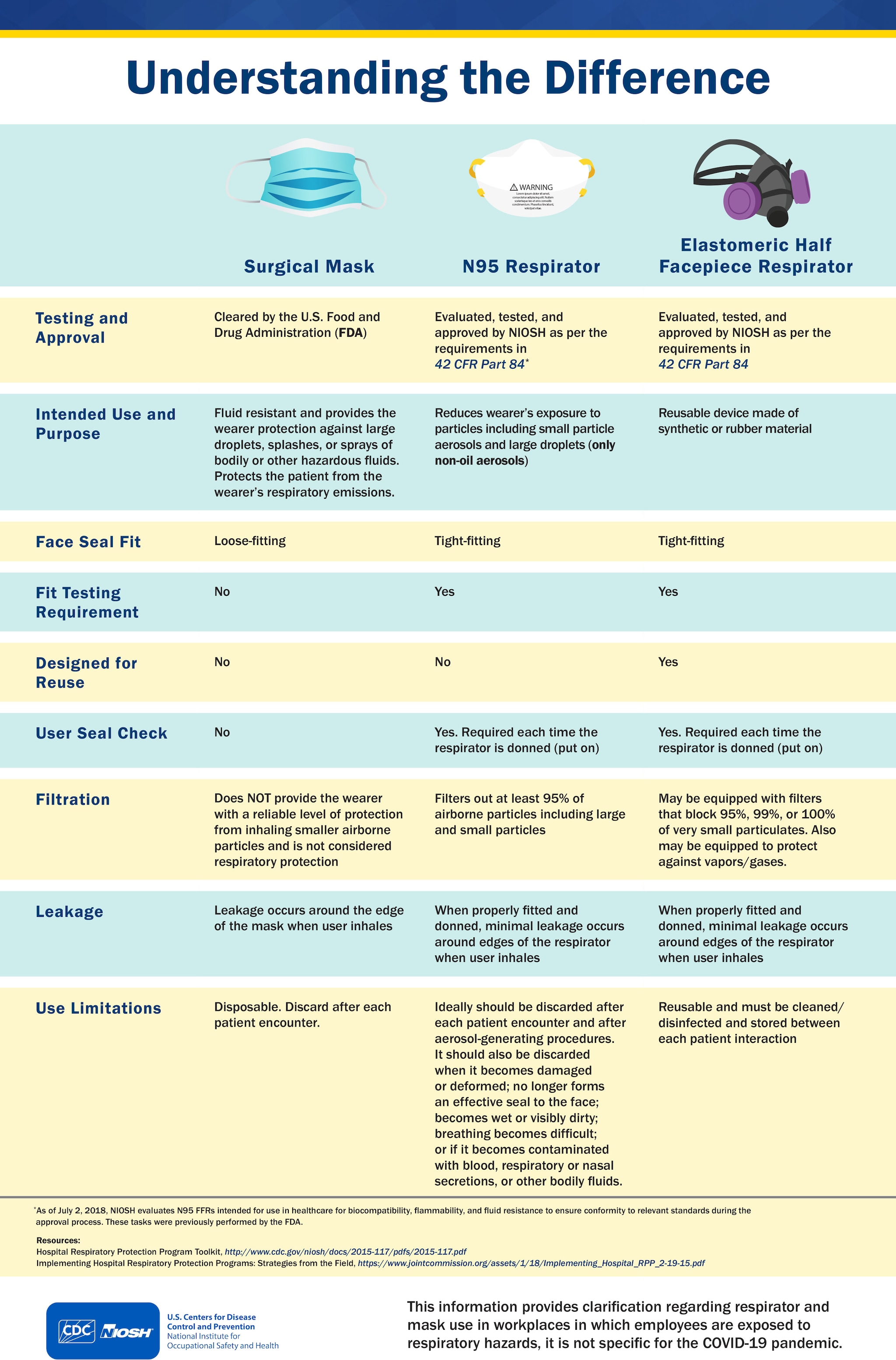
Surgical Masks
Surgical masks are loose-fitting and disposable. They are designed to create a light but effective physical barrier between your mouth and nose and any potential contaminants in the environment. Surgical masks are often broadly referred to as “face masks,” but not all face masks are regulated as surgical masks.4
Surgical masks come in various forms and thickness to protect against contact from liquids without hampering your ability to breathe. When worn properly, surgical masks can effectively keep out:
- Large-particle droplets
- Sprays
- Splashes4
They can also reduce exposure to saliva and other respiratory secretions from another person. However, they may be less in filtering out smaller particles, transmitted by cough or sneeze. 4
That does not make surgical masks completely useless against COVID-19. In a study, researchers looked at the effectiveness of surgical masks against influenza bioaerosols. Several surgical masks designs were used in conjunction with a dummy head attached to a breathing simulator. The researchers measured the levels of inert particles in front of and behind the masks. Results of the study found that live influenza virus particles were measurable behind every mask, but the surgical masks still reduced overall exposure to aerosols. The exact reduction varied based on the design, but on average, the reductions measured 6-fold. Even at the low end, surgical masks reduced exposure by 1.1-fold, while at the high end, reductions measured 55-fold.5
Surgical masks won’t provide complete protection, but they may still be helpful. However, they are meant to be disposed of after a single usage, and they should not be shared or reused.4
Cloth Masks
Cloth masks are simple masks usually made from simple cotton. These are generally ineffective at blocking or filtering out droplets. In one of the few randomized controlled trials comparing cloth masks to surgical masks, researchers found that the rate of influenza-like illness was significantly higher in cloth mask groups than in both surgical mask and control groups. Particle penetration was about 97 percent for cloth masks, while surgical masks had a 44 percent penetration rate. The increased risk of infection may come from moisture retention, poor filtration, and the fact that the cloth masks were reused every day over the course of four weeks.6
In another study, researchers compared the effectiveness of surgical masks to cloth masks made from cotton t-shirts. Both masks were found to significantly reduce the number of microorganisms expelled by the volunteers, though surgical masks were found to be on average three times more effective than the cloth masks.7
More research is necessary to determine just how effective cloth masks could be, especially given if everyone in a large population regularly wore masks, but most experts and current research agree that cloth masks are ultimately not as effective as actual surgical masks. However, as a last resort, cloth masks are better than not wearing any protection at all.
N95 Respiratory Face Masks
The N95 respirator is currently the best of the best. It is a respiratory protective device that is efficient in filtering out airborne particulates. Unlike a surgical or cloth mask, N95 respirators are designed to fit tight over the nose and mouth, essentially creating a seal that prevents any particles or air from coming in through the sides of the mask. The “N95” designation refers to their tested ability to filter out 95 percent of microbes and particles measuring just 0.3 microns in diameter.4
The key here is the filtration itself, which comprises a dense tangle of filaments. This prevents a direct line through the mask. Instead, particles have to pass through a maze-like series of obstructions while also traveling with the natural air currents. Larger particles are unable to pivot and turn quickly, forcing them to get stuck in the filaments, but smaller particles have to contend with individual air molecules that bounce and collide with the particles and filaments. While a particle or viral microbe that is 0.3 microns could potentially get through, the amount of twists and turns essentially makes it difficult.1
Similar to surgical masks, the N95 respirator is not meant for reuse. Once they become wet, dirty, or damaged, they are meant to be disposed of properly.
Surgical Masks vs. N95 Respirators
To be completely effective, N95 respirators have to be properly fitted, sometimes even custom fitted, to ensure a tight seal around the nose and mouth. This can be uncomfortable, but for most medical professionals and healthcare workers, N95 masks are the best option.
However, given the current supply shortages, surgical masks should not be ignored. In one randomized trial, nurses in eight tertiary care hospitals in Ontario were studied to compare the effectiveness of N95 masks and surgical masks during influenza season. Results of the study found that 23.6 percent of nurses in the surgical mask group experienced an influenza infection, while 22.9 percent of nurses in the N95 respirator group experienced an influenza infection. This suggests that surgical masks should not necessarily be considered inferior to the N95 respirator.8
Another study, this time involving patients with influenza, found similar results. A group of 26 patients diagnosed with influenza were enrolled in an eight-week study where they coughed without a mask, coughed while wearing a fitted N95 mask, coughed while wearing a surgical mask, and coughed again without a mask. Results of this study found that both surgical and N95 masks were equally effective in filtering influenza virus and preventing its spread from a coughing patient.9
However, these studies did not specify which grade of surgical masks were used. Surgical masks actually have different kinds of ratings based on how much they can filter out. ASTM level 1 masks with a Viral Filtration Efficiency (VFE) greater than or equal to 95%. This means that a level 1 mask can filter out 95% of 0.1 micron particles while ASTM level 2 and 3 masks have a VFE greater than or equal to 98%. Level 2 and Level 3 masks can filter out more than 98% of particles 0.1 microns or bigger.13 The average diameter of a coronavirus is around .12 microns11 so they are filtered out by surgical masks.
When choosing a surgical mask, ensure that it has a VFE rating to filter out viral particles. We will go over more details about the different grades of surgical masks in a later article.
Reusable Elastomeric Respirators
Reusable respirators are another solution that health care workers who are constantly exposed to aerosolized pathogens should consider. These masks are made of plastic and utilize silicone to form a comfortable seal. They are washable and the filter elements are replaceable. In the healthcare setting these masks can be reused, washed, and the filters need to be replaced only after 1 year of usage.
A tuberculosis hospital in Texas found that 40-50% of their staff developed an immune reaction to tuberculosis (as determined by the tuberculin skin test, or TST) when using medical masks and 1-2% had tuberculosis disease after being employed by the hospital.
Since the hospital decided to switch to reusable elastomeric respirators in 1994, no employees have been exposed to tuberculosis as determined by TST testing.12 This means that reusable elastomeric respirators are excellent in cases of pandemics where traditional disposable masks are in short supply such as the current crisis. However, these masks should be reserved for healthcare workers who are constantly exposed to infectious diseases.
Should People Wear Face Masks?
When used properly, face masks can significantly reduce the risk of exposure and prevent the spread of COVID-19. While the size of particles does matter, any microbes expelled from a person’s respiratory tract don’t come out on their own. Respiratory droplets range from 0.6 to over 1,000 microns.10 Any sort of mask can still act as a significant impediment to these droplets.
At the same time, it’s important to remember that no mask will completely block out any particle or virus. The global pandemic caused by the novel coronavirus has been unprecedented, and even experts still have much to learn about the virus and its potential means of transmission. Face masks are effective, but they are not a replacement for other forms of intervention. They should be used in conjunction with other healthy practices, including proper social distancing, hygiene, and regular disinfecting.1
Although face masks can play an integral role in preventing infection and slowing the spread of COVID-19, the United States is currently experiencing a mass shortage of face masks and other forms of personal protective equipment (PPE). This has led to dire problems for those who are more vulnerable to the virus (the elderly and immunocompromised) as well as the thousands of healthcare professionals putting their lives on the line every single day to help those affected by COVID-19.
While it would be ideal for everyone to wear a face mask when going out in public, that is just not possible right now. Until the supply numbers normalize, the best course of action currently is to continue to practice safe social distancing and wash your hands frequently. Above all, do not hoard face masks, which takes resources away from those who need them the most. Instead, consider sewing face masks for germs of your own or donating to local organizations who are providing PPEs for medical professionals.
CDC Face Masks Recommedations
Sources:
- https://www.wired.com/story/its-time-to-face-facts-america-masks-work/
- https://jamanetwork.com/journals/jama/fullarticle/2763852
- https://academic.oup.com/annweh/article/52/3/177/312528
- https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-and-surgical-masks-face-masks
- https://www.sciencedirect.com/science/article/abs/pii/S0195670113000698
- https://bmjopen.bmj.com/content/5/4/e006577.short
- https://www.ncbi.nlm.nih.gov/pubmed/24229526
- https://jamanetwork.com/journals/jama/article-abstract/184819
- https://academic.oup.com/cid/article/49/2/275/405108
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2894888/
- https://pubmed.ncbi.nlm.nih.gov/25720466/
- https://www.nap.edu/catalog/25275/reusable-elastomeric-respirators-in-health-care-considerations-for-routine-and
- https://www.nelsonlabs.com/testing/surgical-face-masks-and-general-use-masks-astm-f2100/



